Research Results
Momentous first step toward regenerative medicine using iPS cells!
Successful iPS cell transplant surgery on a human! FY2017

- Masayo Takahashi (Project Leader of the Laboratory for Retinal Regeneration, RIKEN Center for Developmental Biology)
- Strategic Promotion of Innovative Research and Development (S-Innovation)
- Construction of Medical Industry Using Cells with iPS at Its Core
"Retinal Regeneration by Cell Transplantation" Project manager (2009-2011) - Highway Program for Realization of Regenerative Medicine
- "Development of Age-Related Macular Degeneration Treatment by the Transplantation if iPS Cell-Derived Retinal Pigment Epithelium Cells"Project leader (2011-2015) *
*This project has been transferred to the Japan Agency for Medical Research and Development as of April 1, 2015.
Seven years since stunning debut; milestone leading to practical application
It was on September 12 in 2014, seven years from when Professor Shinya Yamanaka sent shock waves through the world with the establishment of iPS cells, that the operation in which a patient's own iPS-cell derived retinal pigment epithelium (RPE) cells were transplanted into the same patient with exudative age-related macular degeneration was performed.
This was the world's first case where tissue produced from iPS cells was used in a transplant surgery on a human.
What is exudative age-related macular degeneration?
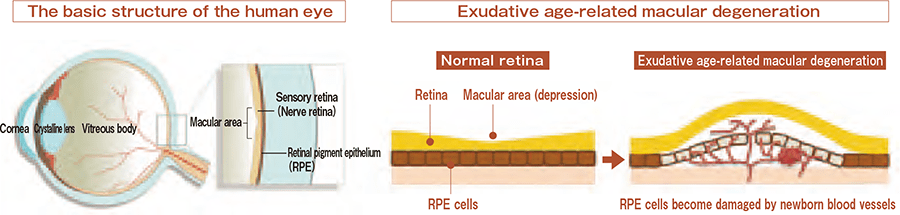
The retina consists of the sensory retina containing visual cells (neural retina) and the retinal pigment epithelium(RPE). The RPE is responsible for nutritional support to nerve cells and the digestion of waste.
When the RPE and the sensory retina become damaged by abnormal blood vessels called choroidal neovasculars, the function of the macular area deteriorates.
Even a huge wall is to be overcome someday
The center of an eye retina is called the macula, which plays an important role when you see things. Exudative age-related macular degeneration is a disease in which abnormal blood vessels are newly generated under the retina in the macula area. This disease leads to the deterioration of vision, and before long, results in the loss of sight. Although the cause of the disease has yet to be understood in detail, this disease is considered to be associated with the aging of RPE cells. Therapeutic agents to suppress the development of blood vessels have been developed; however, it is still impossible to undo the damage in RPE cells and tissue with such therapeutic agents. For a radical cure, the transplantation of RPE cells is necessary.
Project Leader Masayo Takahashi proceeded with the study of inducing differentiation of ES cells (embryonic stem cell), which are pluripotential stem cells derived from reproductive cells, into RPE cells, and produced good results; however, the use of ES cells was not approved in Japan due to problems associated with the regulations. Thus, the establishment of the technique to induce the differentiation of ES cells into RPE cells did not go far enough in opening the way to its practical use.
Becoming a frontrunner leading to the practical use of iPS cells
That was when iPS cells appeared like a savior. Since being able to be produced from a patient's own cells, the use of iPS cells doesn't pose grave ethical problems and doesn't carry a serious risk of rejection. Project Leader Takahashi says: "I felt like I had seen a ray of light in the darkness." Then she became a research leader of the Strategic Promotion of Innovative Research and Development, and since then, started to work on the establishment of the technique to induce the differentiation of ES cells into RPE cells and its clinical application. Fortunately, the di erentiationinducing method to be used for iPS cells was found to be not signi cantly di erent from that used for ES cells, so the research advanced steadily. Among the researches on regenerative medicine associated with iPS cells that started around the same time, the research conducted went one step further ahead of what the others were doing, attracting attention as a pioneer in the practical uses of iPS cells.
After the Highway Program for Realization of Regenerative Medicine that was based on the New Growth Strategy started in 2011, the research was adopted as the research subject for the aforementioned program under the name of the Development of Age- Related Macular Degeneration Treatment by the Transplantation of iPS Cell-Derived Retinal Pigment Epithelium Cells, thus the research further accelerated. In July 2013, the Ministry of Health, Labour and Welfare approved its clinical research implementation plan, and the clinical research finally started.
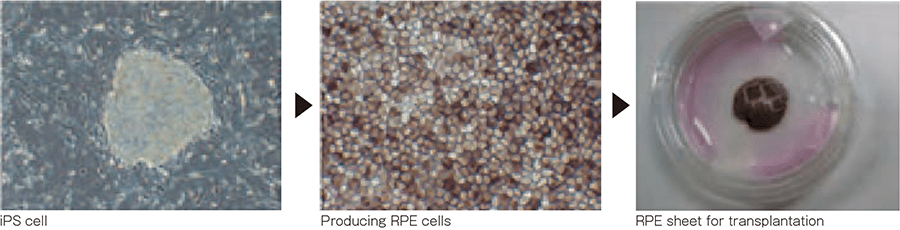
Producing RPE cells from iPS cells
Great significance of the "first step"
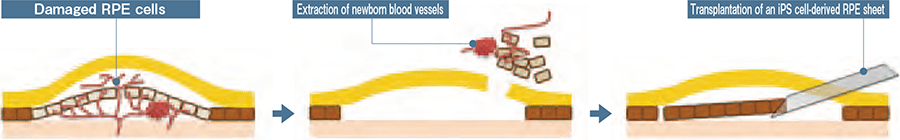
Prior to the transplant surgery, skin tissue was taken from the patient's arm, and then it was cultured to produce iPS cells. After that, the produced iPS cells were induced to differentiate into forming RPE cells, from which a sheet the size of 1.3 mm × 3 mm was produced. On the day of the surgery, the abnormal blood vessels that were constituting a factor for the deterioration of vision were removed and the sheet-liked RPC cells were transplanted. Now, a follow-up inspection is being carried out.
This surgery was performed as part of clinical research at an early stage. The main purpose lay in the confirmation of safety, rather than in achieving a remarkable therapeutic effect such as significant vision improvement. It is necessary to conduct prolonged further clinical research in the future until this therapeutic method is established as a new therapeutic method and becomes common. iPS cells, which sent shock waves through the world, thus took the first step toward bringing a blessing to mankind.
Transplantation of an iPS cell-derived retinal pigment epithelium (RPE) sheet