Research Results
Contributing to R&D of medical products
Organ generation using iPS cells FY2017

- Hideki Taniguchi (Professor, Graduate School of Medicine, Yokohama City University)
- S-Innovation
- "Constriction of human hepatic stem cell library for pharmaco-cellomics" Program manager (2009-2013)
- Regeneration medicine realization hub network program
- "Hub for development of generation of metabolic organs using iPS cells" manager (2013-)*
*This research project has been transferred to the Japan Agency for Medical Research and Development as of April 1, 2015.
iPS cell research - the next step in "clinical research" and "organ generation"
In November 2007, a research team (Professor Shinya Yamanaka et al., Kyoto University) generated "iPS cells" from cutaneous cells. This research surprised the world, because it had been generally believed in the medical world that it was impossible to reprogram cells once they differentiated. However, the "iPS cells" have pluripotency which allows them to differentiate into any type of cell.
Now researchers have almost completed the research stage regarding what types of cells iPS cells can differentiate into. The main themes presently being addressed are "Clinical research developed by the application of iPS cells" and "Organ generation." These two themes correspond with the application of the iPS cells in regenerative medicine, or medical treatment for regeneration of lost tissues and organs. In 2013, researchers made substantial progress in these areas. As for the former theme, Project Leader Masayo Takahashi et al. in RIKEN, launched the first clinical research in the world in the regeneration medicine realization hub network program that took on the results of s-innovation in August 2013. As for the latter theme, Professor Hideki Taniguchi with his team members at Yokohama City University generated a human organ in s-innovation for the first time in the world in July.
Perceptional change "from cell induction to organ induction"
There is a disease that is called "terminal organ incompetence." If a person suffers from this disease, his/her specified organ fails to function. An effective medical treatment for this case is "organ transplantation", in which a healthy organ is replaced with a damaged organ. However, organs from donors are in extremely short supply while the number of patients who need an organ transplant are increasing year after year. Thus, in order to solve this problem, it is urgent and imperative to develop a medical treatment which will serve as a substitute for organ transplantation. For this reason, researchers have recently carried on the regenerative medical research, using differentiated and inducted organ cells from pluripotent stem cells (iPS cells, ES cells) with the aim of recovering damaged organ function.
In order to achieve this, the research group of Professor Hideki Taniguchi et al. departed from the previous developmental notion of "cell differentiation induction." Instead, the group aimed to realize "differentiation and induction based on organ reconstruction." Naturally, organs are constructed not only with cells that bear a specific function (functional cell), but also with multiple kinds of cells which are arranged three-dimensionally and interact with one another, both of which contribute to the proper function of the organ. Thus, the basic idea can be described as follows: in order to acquire cells that function fully, it is imperative to"induce organs" (organ generation) that enable the reconstruction of three-dimensional tissues, in addition to inducing the differentiation of the functional cells.
The way the iPS cells become human livers
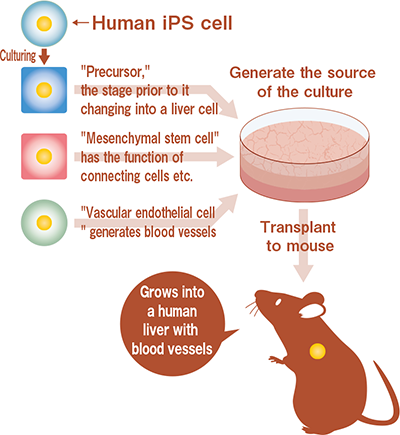
3 types of cells gathered together in a ball shape to create a "mini-liver"!
First of all, the research group developed a new cell culture handling technique in order to follow the process of "organ rudiment" (organ seed) formation that takes place in the womb in a test tube. After this, the research group added "vascular endothelial cells" (that generated blood vessels) and "mesenchymal stem cells" (that had the function to connect cells) to "endoderm cells" that were made of human iPS cells ("precursors" that are in the stage just before they differentiate into liver cells), then co-cultured in a test tube. As a result, 3 types of undifferentiated cells gathered together in a ball shape to form autonomously three-dimensional liver rudiments (what is called the human "mini-liver") in approximately 48 hours. When they transplanted these rudiments to living organisms (immunosuppressed mice), vascular networks with bloodstreams were reconstructed, and finally it was found that the rudiments matured into tissue with features of human liver functions, such as synthesis of protein and drug metabolism. In addition, the survival rate of the mice group that had the hepatic failure, into which the rudiments had been transplanted, improved significantly compared to the mice group that didn't received the transplantation. This indicates that human liver cells that were differentiated and inducted in living organisms were successful in performing a function as a liver, and the effectiveness of the treatment was observed.
Thus, this research group succeeded in creating a functional human liver with vascular networks from iPS cell-derived cells for the first time in the world.
Picture of the formation process for the human liver rudiment in three-dimension
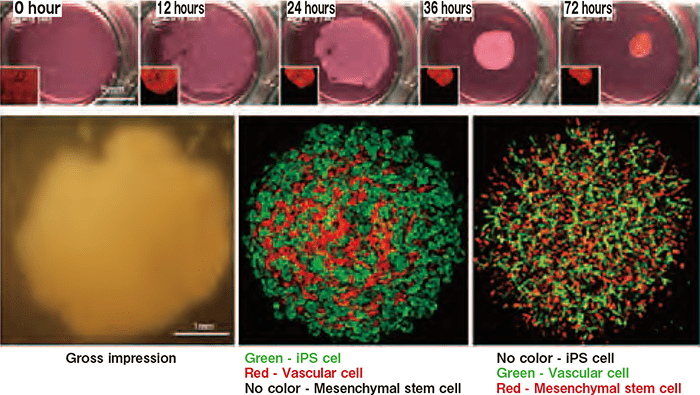
By co-culturing 3 types of undifferentiated cells under special conditions, three-dimensional liver rudiments were formed autonomously (upper). It became obvious that iPS cell-derived endoderm cells can be differentiated and inducted into liver precursors effectively, and vascular cells can also form network-like structures (lower)
For alternate treatment of organ transplant and pharmaceutical screening
The research group of Professor Taniguchi et al. named this developmental technique as a "transplant remedy for organ rudiment," and proposed this remedy as an alternate treatment for organ transplants. If we can substantiate the treatment based on the technique, we will be able to save the lives of many patients. To that end, the research group is now working on mass producing technology, seeking the best way to transplant organ rudiments, trying to realize the regenerative medicine for patients with liver disorder, and thus accelerating the research for the application possibility for organs other than the liver.
On the other hand, the result of this research is likely to contribute largely to the development of the pharmaceutical industry in Japan. Human hepatic cells are regarded as highly marketable and the most important among the cells currently utilized for the development in the pharmaceutical industry. They have proved to be useful for screening (selection of new drug candidates) for pharmaceutical developments such as metabolic stability tests and enzyme induction, but unfortunately, almost 100% of the supply relies on Europe and the United States at present. Therefore, we believe that if we are able to produce iPS cell-derived human hepatic cells and hepatic tissues in large quantity and provide them for the screening using the technique developed through this research, we will make a further contribution to the development in the pharmaceutical industry in Japan.
